 (Dec. 5, 2017) The ME/CFS Collaborative Research Center at Stanford will be led by Dr. Ron Davis, Professor of Biochemistry and Genetics at Stanford University, and Director of our Scientific Advisory Board. Dr. Davis has assembled a truly world-class team of researchers, many of whom have never before focused their expertise on ME/CFS, and has planned several innovative projects that will help us to understand the molecular basis of ME/CFS, develop better diagnostics, and discover new treatments. Given the number and quality of investigators that this grant would bring into the field, and the likelihood of groundbreaking discoveries coming from this research, OMF has decided to fund this highly promising proposal. Although the National Institutes of Health decided against funding this plan as one of their Collaborative Research Centers, we believe this work is too important and too promising not to pursue. We are not willing to miss the opportunity to actively involve a scientific team of this caliber in the field of ME/CFS research. OMF will, therefore, be supporting the first year of this groundbreaking research with $1.2 million, and we are actively and enthusiastically raising the funds needed to support the remaining 4+ years it will take to complete it.
(Dec. 5, 2017) The ME/CFS Collaborative Research Center at Stanford will be led by Dr. Ron Davis, Professor of Biochemistry and Genetics at Stanford University, and Director of our Scientific Advisory Board. Dr. Davis has assembled a truly world-class team of researchers, many of whom have never before focused their expertise on ME/CFS, and has planned several innovative projects that will help us to understand the molecular basis of ME/CFS, develop better diagnostics, and discover new treatments. Given the number and quality of investigators that this grant would bring into the field, and the likelihood of groundbreaking discoveries coming from this research, OMF has decided to fund this highly promising proposal. Although the National Institutes of Health decided against funding this plan as one of their Collaborative Research Centers, we believe this work is too important and too promising not to pursue. We are not willing to miss the opportunity to actively involve a scientific team of this caliber in the field of ME/CFS research. OMF will, therefore, be supporting the first year of this groundbreaking research with $1.2 million, and we are actively and enthusiastically raising the funds needed to support the remaining 4+ years it will take to complete it.
Scientific Plan
The Center will pursue three distinct projects, all related to understanding and treating ME/CFS by developing and using cutting-edge technologies. This work will build on previous projects that OMF has supported. For more information about these projects from the scientists involved, please see the YouTube videos from our recent Community Symposium on the Molecular Basis of ME/CFS.
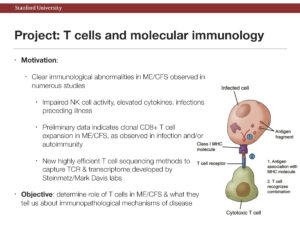
1. T cells and the molecular immunology of ME/CFS
Sequencing single T cells and discovering their targets
Many studies have shown that the immune system is affected in ME/CFS patients, e.g., low activity of NK cells, altered levels of cytokines (signaling molecules of the immune system), and the likelihood of a microbial infection preceding the illness. Now, scientists on this team have implicated T cells – the immune cells responsible for identifying and killing infected cells – in ME/CFS. Specifically, their discovery of T cell clonal expansion indicates that patient T cells are reacting to a foreign invasion (e.g., virus) and/or to the ‘self’ (autoimmunity). HLA genes play a part in this reaction, and personal variations in these genes may also be playing a role in the risk of developing the disease. Discovering what is triggering this T cell clonal expansion will help to determine immunological causes of ME/CFS, may explain the elevated cytokine levels, and could lead to new treatments.
The Collaborative Research Center at Stanford will investigate the immunological basis of ME/CFS using several approaches. Dr. Mark Davis’ team will investigate the clonal expansion of T cells in ME/CFS, including what they might be targeting – viruses, bacteria, or self (autoimmune). Dr. Ron Davis’ team has invented a highly accurate, cost-effective method for HLA gene sequencing and a very sensitive method for detecting viral DNA as a sign of viral infections, which he will use in this project. Dr. Lars Steinmetz’ team has developed effective methods for sequencing RNA from single T cells, which they will use to understand how T cell behavior may be different in ME/CFS. Overall, these methods will help to determine if ME/CFS is an autoimmune disease, and what immune factors may be triggering ME/CFS or sustaining it as a chronic disease. By helping to understand the immunology of ME/CFS, it may be possible to identify treatments that modulate the immune response.
2. Extended big data study in families
Genome sequencing, gene expression, metabolomics, cytokines, clinical features, and more
OMF has funded a big data study of 20 severely ill ME/CFS patients, encompassing a huge variety of molecular and clinical tests, the largest of its kind in this disease. Among many things, this study is helping to look for genetic factors and potential molecular biomarkers, and is allowing us to generate many hypotheses. The analysis of this data set, led by Dr. Wenzhong Xiao, has yielded many interesting observations, but it is clear that more patients must be profiled in this way to validate and extend these observations to a less severe population. The Collaborative Research Center at Stanford will expand this big data study to patients of varying severities and their families.
 It has been clear for some time that there are families with multiple members affected. This might be caused by a genetic predisposition to the disease. Studying these families is likely to yield a better understanding of the factors that make someone susceptible to ME/CFS. Fereshteh Jahanbani, PhD, a Research Associate with Mike Snyder, PhD, hypothesizes that using unaffected members of these families as controls will reduce the variance in the data between controls and affected, because of the similarities in their genetics, environment, and diet. The team anticipates that this study will help define meaningful subgroups of patients, biomarkers that could be useful in diagnosis and monitoring of disease progression, and molecular defects that could be targeted with new treatments.
It has been clear for some time that there are families with multiple members affected. This might be caused by a genetic predisposition to the disease. Studying these families is likely to yield a better understanding of the factors that make someone susceptible to ME/CFS. Fereshteh Jahanbani, PhD, a Research Associate with Mike Snyder, PhD, hypothesizes that using unaffected members of these families as controls will reduce the variance in the data between controls and affected, because of the similarities in their genetics, environment, and diet. The team anticipates that this study will help define meaningful subgroups of patients, biomarkers that could be useful in diagnosis and monitoring of disease progression, and molecular defects that could be targeted with new treatments.
3. Developing blood-based diagnostic and drug screening technology
Enabling fast, inexpensive diagnosis of ME/CFS and discovery of new treatments
One of the greatest obstacles in ME/CFS research and patient care is the lack of a biological diagnostic. Dr. Davis’ engineering team has promising preliminary technologies that can distinguish ME/CFS blood samples from healthy samples, and is currently refining these technologies and investigating what the results tell us about ME/CFS biology. The technologies include the nanoneedle biosensor, developed by Rahim Esfandyarpour, PhD, the magnetic levitation platform developed by Gozde Durmus, PhD, and more. The Collaborative Center will continue this work to engineer a blood-based diagnostic device that would also be useful as a reporter for drug screening. Dr. Davis’ team has already tested chemicals in two of our platforms, some of which have made the patient samples behave more like healthy samples. To validate these findings and test large numbers of samples and candidate drugs, they will further develop and optimize the technology. Eventually, the developed technology will be shared across the ME/CFS research community to accelerate its evaluation and adoption as a clinical diagnostic assay. The Stanford Genome Technology Center has developed a number of diagnostic assays that have been commercially exported and are now in clinical use. Dr. Davis’ team has experience in the complex process of developing and implementing an assay that becomes approved for clinical use, in the USA, as well as in Europe and other countries.
Update Nov 2018: OMF funded Red Blood Cell Deformability research may lead to a biomarker. The abstract was published in Blood Journal.
Update April 2019: OMF funded Research Publication: A Nanoelectronics-blood-based diagnostic biomarker for ME/CFS. The article and abstract were published in PNAS.
Scientific Team
To carry out this ambitious work, Dr. Davis has assembled a team of extraordinary scientists with expertise in a variety of areas directly relevant to ME/CFS research. Most of these scientists are new to ME/CFS, bringing with them extensive knowledge and perspective from other fields and diseases.
ME/CFS Collaborative Research Center at Stanford Team:
Ron Davis, PhD, Professor of Biochemistry and Genetics, Stanford University School of Medicine; Director, Stanford Genome Technology Center; Director, Chronic Fatigue Syndrome Collaborative Research Center at Stanford University; Director, Open Medicine Foundation ME/CFS Scientific Advisory Board.
Mark M. Davis, PhD, Director, Stanford Institute for Immunology, Transplantation and Infection (ITI); Professor of Microbiology and Immunology; Howard Hughes Medical Institute Investigator.
Mike Snyder, PhD, Chair, Stanford Department of Genetics; Director, Stanford Center for Genomics and Personalized Medicine
Wenzhong Xiao, PhD, Director, Immuno‐Metabolic Computational Center, Massachusetts General Hospital, Harvard Medical School.
Craig Heller, PhD, Professor of Biology, Stanford University, exercise physiologist.
Robert Phair, PhD, Chief Science Officer, Integrative Bioinformatics, Inc..
Lars Steinmetz, PhD, Co-Director, Stanford Genome Technology Center; Professor of Genetics, Stanford University; Senior Scientist, Genome Biology Unit, European Molecular Biology Laboratory.
Laurel Crosby, PhD, Engineering Research Associate, Stanford Genome Technology Center – multi-system integration
Rahim Esfandyarpour, PhD, Engineering Research Associate, Stanford Genome Technology Center – electrical engineering, device fabrication
Fereshteh Jahaniani, PhD, Research Associate, Stanford Center for Genomics and Personalized Medicine – multi-omics
Mohsen Nemat-Gorgani, PhD, Life Science Research Scientist, Stanford Genome Technology Center – protein biochemistry, enzymology
Peidong Shen, PhD, Research Associate, Stanford Genome Technology Center – biochemistry, cell-free DNA detection methods
Gozde Durmus, PhD, Postdoctoral Fellow, Stanford Genome Technology Center – magnetic levitation platform, bioengineering
Julie Wilhelmy, Life Science Research Professional, Stanford Genome Technology Center – experimental genomics, immunology
Robert Naviaux, MD, PhD, Professor of Medicine, Pediatrics, and Pathology, University of California, San Diego; Co-Director of Mitochondrial and Metabolic Disease Center
William Robinson, MD, Associate Professor of Medicine (Immunology and Rheumatology), Stanford University
Curt Scharfe, MD, Associate Professor of Genetics, Yale University
Lucinda Bateman, MD, founder and Medical Director of the Bateman-Horne Center for ME/CFS and Fibromyalgia
David Kaufman, MD, ME/CFS Physician
Working Group
We are fortunate that many members of the scientific, medical, and biotechnology communities have offered their expertise and resources to this Center.
Paul Berg, PhD, Professor of Biochemistry, Emeritus, Stanford University; Nobel Laureate
Mario Capecchi, PhD, Professor of Human Genetics and Biology, University of Utah; Nobel Laureate
Baldomero Olivera, PhD, Professor of Biology, University of Utah
Alain Moreau, PhD, Professor of Biochemistry and Molecular Medicine, University of Montreal
Øystein Fluge, MD, Department of Oncology and Medical Physics, University of Bergen, Haukeland University Hospital, Bergen, Norway
Olav Mella, MD, Department of Oncology and Medical Physics, University of Bergen, Haukeland University Hospital, Bergen, Norway
Jonas Bergquist, MD, PhD, Professor of Analytical Chemistry and Neurochemistry, Uppsala University, Sweden
Jonas Blomberg, MD, PhD, Professor of Clinical Virology, Emeritus, Uppsala University, Sweden
Maureen Hanson, PhD, Professor of Molecular Biology and Genetics, Cornell University
Chris Armstrong, PhD, Department of Biochemistry and Molecular Biology; Bio21 Molecular Science & Biotechnology Institute researcher at the University of Melbourne, Melbourne, Australia
Neil McGregor, BDS, MDSc, PhD, senior researcher, Bio21 Molecular Science and Biotechnology Institute, University of Melbourne, Melbourne, Australia; Adjunct Professor, Victoria University, Melbourne, Australia
Ronald Tompkins, MD, ScD, Professor of Surgery, Harvard Medical School; Founding Director of Center for Surgery, Science & Bioengineering at Massachusetts General Hospital
Catherine Blish, MD, PhD, Assistant Professor of Medicine and of Immunology, Stanford University
Christopher Garcia, PhD, Professor of Molecular and Cellular Physiology, Stanford University
Roger Howe, PhD, Professor of Engineering, Stanford University; Director, Stanford Nanofabrication Facility
Tom Soh, PhD, Professor of Electrical Engineering, Radiology, and by courtesy, Chemical Engineering, Stanford University
Robert Tibshirani, PhD, Professor of Biomedical Data Sciences and Statistics, Stanford University
Emmanuel Mignot, MD, PhD, Professor of Sleep Medicine and of Psychiatry and Behavioral Sciences, Stanford University; Director of Stanford Center for Sleep Sciences and Medicine
Gerald Shadel, PhD, Professor of Pathology and Genetics, Yale University; Director of Yale Center for Research on Aging
Jarred Younger, PhD, Associate Professor of Anesthesiology and Rheumatology and of Psychology, University of Alabama at Birmingham; Director, Neuroinflammation, Pain, and Fatigue Laboratory
John Ryals, PhD, President and CEO, Metabolon
Chunlin Wang, PhD, Chief Technology Officer, iRepertoire, Inc.
Michael Mindrinos, PhD, President of Sirona Genomics, an Immucor company
David Bell, MD, ME/CFS Physician
Kevin Tracey, MD, Professor of Neurosurgery and Molecular Medicine, Hofstra Northwell School of Medicine
Jennifer Frankovich, MD, Clinical Associate Professor of Pediatric Rheumatology, Stanford University
Susan Levine, MD, ME/CFS Physician
Harry Greenberg, MD, Senior Associate Dean of Research, Professor of Medicine, Stanford University
Bela Chheda, MD, ME/CFS Physician
Patient partners
We are very grateful for the support and contributions of the ME/CFS patient community, which has and will continue to play an integral role in moving research forward. We are committed to continuing to involve patients as participants and consultants throughout these projects, and maintaining open communication about our findings through a variety of venues. We are especially grateful to all the patients who selflessly volunteer to be subjects in our research, who generously donate to make our research possible and who send Dr. Davis their ideas, scientific analyses, and links to publications. Our patient partners are a significant and essential part of our team.


